Premature sexual development of a girl. What determines premature puberty in children Premature puberty causes
Premature sexual development in girls is classified into:
- true, present - the presence of an increase in the mammary glands, hair growth of the pubis and axillary fossa and menstrual bleeding.
- false - the presence of growth of the mammary glands and adrenarche (the beginning of the secretion of androgens by the adrenal cortex) in the absence of menstruation.
- incomplete - the appearance of only the growth of the mammary glands or the secretion of androgens by the adrenal glands without accelerating body growth and without menstruation.
Reasons for true premature puberty in girls:
1. Idiopathic early sexual development is caused by premature impulse secretion of gonadoliberin - a hormone of the hypothalamus that stimulates the release of gonadotropins by the pituitary gland - follicle-stimulating (FSH) and luteinizing (LH) hormones, which in turn stimulate the secretion of female sex hormones.
2. Some diseases cause excessive secretion of the gonadoliberin, gonadotropins mentioned in the previous paragraph, or their dysregulation in the hypothalamic-pituitary system.
- tumors pituitary gland and the hypothalamus,
- brain damage: trauma, encephalitis, meningitis, the effects of ionizing radiation, chemical factors,
- malformations of the central nervous system and congenital neurological disorders,
- hydrocephalus,
- delayed treatment of adrenogenital syndrome.
Causes of false premature puberty in girls:
1. Isosexual premature sexual development (with an excess of female sex hormones estrogen):
- estrogen-secreting ovarian tumors,
- estrogen-secreting adrenal tumors,
- iatrogenic (due to the use of estrogen or gonadotropin preparations).
2. Heterosexual premature sexual development (with an excess of male sex hormones androgens):
- androgen-secreting ovarian tumors,
- androgen-secreting adrenal tumors.
Causes of incomplete premature puberty in girls:
1. Premature growth of mammary glands.
2. Premature onset of androgen secretion by the adrenal cortex.
Diseases accompanied by accelerated sexual development in girls:
1. Ovarian cysts.
2. Primary hypothyroidism (lack of thyroid hormones due to a pathological process or surgical removal), which is accompanied by hypersecretion of pituitary gonadotropic hormones that stimulate the ovaries, and hypersecretion prolactinwhich affects the growth of the mammary glands.
3. Autonomous ovarian hyperfunction (McCune's syndrome - Albright).
4. Hypersecretion of gonadotropins (Russell-Silver syndrome).
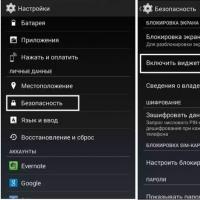
Diagnosis of premature sexual development in girls.
The diagnosis of idiopathic premature sexual development, which occurs as a result of impulsive secretion of gonadoliberin and is manifested by the presence of regular menstruation and the absence of neurological, mental disorders, is established after excluding all pathological causes of premature sexual development.
With true premature sexual development, the presence of a small time interval between the onset of breast enlargement, the appearance of hair growth and the onset of menstruation is found. Normally, 1.5-2 years pass from the initial manifestations of sexual development to the first menstruation, and when this period is shortened to 0.5-1 years, pathological causes of premature sexual development should be sought. Laboratory tests show elevated levels of the luteinizing hormone LH, the follicle-stimulating hormone FSH, in the blood. To detect a tumor, a computed tomography CT scan or magnetic resonance imaging MRI is prescribed.
With false premature sexual development, an increase in the concentration of LH, FSH, thyroid-stimulating hormone TSH, as well as estrogens (due to the autonomous hypersecretion of the latter by the ovaries, adrenal glands, the use of estrogens, choriogonin, primary hypothyroidism) is revealed. The presence of tumors is detected by CT, MRI.
Heterosexual premature sexual development in girls appears in puberty with signs of androgenization in the form of hirsutism (excessive hair growth), acne, accelerated growth, signs of a male physique, coarsening of the voice and clitoral hypertrophy, and the presence of genitalia of an undefined type.
Adrenose-secreting tumors, virilizing forms of adrenogenital syndrome are diagnosed using ultrasound, CT or MRI of the pelvic organs and adrenal glands, as well as by examining blood levels of LH, FSH, ACTH (adrenocorticotropic hormone pituitary gland), cortisol, testosterone, dehydroepiandrosterone, dehydroepiandrosterone sulfate DEA-S.
Treatment of premature sexual development in girls.
With incomplete premature sexual development, which is manifested only by the growth of the mammary glands or the secretion of androgens by the adrenal glands without accelerating body growth and without menstruation, treatment is not carried out, the patient is under annual dispensary observation. In the idiopathic form, androkur and gonadoliberin antagonists are prescribed. With adrenogenital syndrome, glucocorticoids are used. Tumors of the brain, ovaries, adrenal glands are subject to surgical removal.
False PPR
False or LH-RH-independent PPR is understood as the development of secondary sexual characteristics associated with autonomous excess production of steroids by the adrenal glands and gonads. The most common cause of this form of PPD is congenital adrenal cortex dysfunction (ADCD). Less commonly, hormonally active tumors originating from the above-named organs, as well as tumors secreting hCG (chorionepitheliomas, hepatomas, teratomas).
Congenital dysfunction of the adrenal cortex is a group of autosomal recessive hereditary diseases caused by genetic defects in steroidogenesis enzymes. The main link in pathogenesis is a violation of the synthesis of cortisol and / or aldosterone. Permanent cortisol deficiency, based on the principle of negative feedback, stimulates the secretion of adrenocorticotropic hormone (ACTH), which causes hyperplasia of the adrenal cortex, which produces excess androgens.
In the overwhelming majority of cases, there is a deficiency of the enzyme 21-hydroxylase, 10 times less often - a deficiency of 11β-hydroxylase. Currently, numerous point mutations of genes have been found that determine one or another deficiency, correlating with the clinical picture of gluco- and mineralocoticoid insufficiency and severe virilization.
At birth, the external genital organs of girls have a heterosexual structure: varying degrees of hypertrophy of the clitoris, the spliced \u200b\u200blabia majora resemble the scrotum, forming a single urogenital opening at the base of the clitoris (urogenital sinus).
The formation of the external genital organs in boys is isosexual: the penis is enlarged, the scrotum is wrinkled and pigmented, and erections appear early. In the first years of life, due to the anabolic action of androgens, children grow rapidly, they develop skeletal muscles, a coarse voice, male-pattern hair growth on the face, chest, abdomen, and limbs. In persons of both sexes, the differentiation of the skeleton is significantly accelerated.
With a deficiency of aldosterone, the disease is acute. The disease manifests itself from the first weeks after birth and poses a serious threat to health. Clinically, this form is characterized by vomiting, dehydration, and a decrease in blood pressure (BP). The amount of sodium in the blood decreases and potassium increases, the level of renin is high.
With a deficiency of 11β-hydroxylase, along with the symptoms described above, an increase in blood pressure is detected, which can complicate the course of the disease. Girls in prepubertal and puberty have no secondary female sex characteristics and menstruation.
In the blood, the level of renin is lowered, and sodium can be increased.
Hormonal diagnosis is based on the determination of the level of 17-hydroxyprogesterone. With 21-hydroxylase deficiency, it is many times higher than normal values. In patients with 11β-hydroxylase deficiency, the increase in 17-hydroxyprogesterone is less.
The main goal of treatment is to suppress excess ACTH production. For this purpose, the selection of glucocorticoids or together with mineralocorticoids is carried out.
Van Wyck-Grombach syndrome occurs in children with long-term undiagnosed primary hypothyroidism. By the time the symptoms of PPD appear, children have a classic picture of severe hypothyroidism: chondrodystrophic physique, significant growth retardation, muscle hypotonia, low, rude voice, delayed psychomotor development.
The diagnosis was confirmed by low levels of thyroid hormones (T3 and T4) and a sharp increase in the content of thyroid stimulating hormone of the pituitary gland (TSH).
In girls, the first signs of PPD are enlargement of the mammary glands, in some with lactorrhea, the appearance of menarche. Adrenarche (pubic and axillary hair growth) is uncharacteristic. All patients showed high levels of prolactin, as for gonadotropins (LH and FSH), they increased moderately. With ultrasound examination (US) of the small pelvis, polycystic ovaries are visualized in all cases.
A feature of the PPR clinic in boys with this syndrome is a moderate increase in testicles with a weak androgenization of the body, which corresponds to a moderate increase in testosterone levels.
In both sexes, bone maturation lagged behind biological age.
Substitution therapy with thyroid drugs reverses the symptoms of PPR.
Androgen-secreting adrenal tumors (androsteromas) are usually referred to as adrenocarcinomas. They are rare in children. In early adolescence, the incidence of adrenocarcinomas increases in children with Wiedemann-Beckwith syndrome (visceromegaly, macroglossia, hemihypertrophy) and Li-Fraumeni syndrome (multiple malignant neoplasms).
In children with adrenocarcinomas, abnormal expression of tumor markers and a decrease in the expression of factors suppressing tumor growth, the genes of which are localized on the long arm of chromosome 11, were revealed. Anomalies of this chromosome are detected in most patients with adrenocarcinoma.
Boys have a clinical picture according to the type of isosexual sexual development: muscle mass increases, growth rate, secondary hair growth, erections appear, and the timbre of the voice changes. However, the volume of the testicles does not increase.
In girls, signs of virilization are found: apocrine glands (sweat, sebaceous, hair follicles) are activated, body weight increases due to muscle tissue, and the clitoris is hypertrophied. Boys and girls are growing faster.
Estrogen-producing adrenal tumors (corticoestromas) are very rare in children. In girls, in this case, they proceed according to the type of isosexual PPR, and in boys in the clinic, gynecomastia is the leading symptom.
In the study of the hormonal profile, an increase in the level of dehydroepiandrosterone sulfate (DHEA-S) and juvenile levels of LH and FSH are characteristic. In some cases, the concentration of testosterone, estradiol increases. In the diagnosis of adrenal tumors, ultrasound is used.
Steroid-secreting gonadal tumors are rare in childhood. In older girls, arrhenoblastomas (malignant tumors) are found, located in the cortical layer or hilum of the ovary. Undifferentiated tumors have a more pronounced virilizing effect, while differentiated ones have both a weak masculinizing and feminizing effect. Granulosa cell tumor of the ovary, often of benign genesis, secretes a large amount of estrogen, causing isosexual PPR. Excess estrogen causes menstrual syndrome - from scanty to profuse bleeding, pigmentation of the areoles, thickening of the glandular tissue, hypertrophy and swelling of the vulva. The amount of estradiol is dramatically increased with pre-pubertal LH and FSH.
Testosterone-secreting leydigomas are rare in boys. It is a benign tumor that affects one testicle. Outwardly, it is enlarged, bumpy, of dense consistency. Androgenization syndrome develops rapidly.
Sertolioma is a neoplasm containing Sertoli cells. In this case, the release of estradiol into the blood increases, which forms gynecomastia in boys, accelerates growth and bone maturation.
The level of gonadotropic hormones in both testicular tumors corresponds to the age of the children.
Follicular ovarian cysts are a common cause of PPR in girls. However, they are also found in healthy girls in the prepubertal period. The diameter of these cysts is from 0.5 to 1.5 cm. The presence of a cyst in the ovaries is not a sign of pathology. But in some cases, the cystic tissue begins prematurely and overproduces estradiol. Typically, these cysts are 3-4 cm in size. Follicular cysts can be accompanied by irregular scanty secretions from the genital tract, hypertrophy and swelling of the vulvar skin, increased vaginal folds, moderate pigmentation and swelling of the nipples. The size of the uterus and bone maturation correspond to the passport age. The cause of the formation and persistence of follicular cysts may be a transient rise in gonadotropins (mainly FSH). Ovarian cysts are found on pelvic ultrasound. In most cases, follicular cysts spontaneously regress after 1.5-2 months and the PPR clinic disappears. Cysts of large sizes or with complications are subject to surgical treatment.
Incomplete forms of PPR
Isolated premature thelarche (PT) - enlargement of the mammary glands in girls - is the most common benign variant of PPR. In most cases, it is observed at the age of 6-24 months in girls who are breastfed, in low birth weight and premature babies. Less commonly found after reaching 3 years of age.
The reason for the increase in mammary glands is considered to be a high level of gonadotropic hormones (especially FSH). Peak FSH concentration after birth persists for up to 6 months and then slowly begins to decline by 2–3 years. In preschool age, such patients have follicles in the ovaries that reach the size of adult women. Some authors attribute this to dysfunction of the hypothalamic-pituitary system. FSH activates the aromatase enzyme, which leads to increased production of estrogen from testosterone in the granulosa tissue of the follicle. Other causes of isolated thelarche can be periodic releases of estrogen or increased sensitivity of the receptor apparatus of the mammary glands to estrogens.
Enlarged mammary glands are palpable on one or both sides. In some girls, moderate estrogenization of the vulva is noted. There are no other secondary sexual characteristics.
In isolated thelarche, the growth rate is not disturbed (5-6 cm per year), the bone age corresponds to the chronological one. Most often, the process regresses on its own and does not require medical intervention, but at the same time, the appeared thelarche may be the first sign of a true or false PPR, therefore, all girls with thelarche must be re-examined (at least 2 times a year).
If thelarche is combined with accelerated bone age, but there are no other signs of premature sexual development, this condition is assessed as an intermediate form of PPR and requires more careful monitoring (quarterly) with ultrasound control of the ovaries and bone age.
Premature adrenarche (PA) is the appearance of isolated hair on the pubis and / or armpits in girls under 8 years old, and in boys up to 9 years old. It is more common in girls aged 6-8 years. PA may be a variant of the norm, given that the maturation of the reticular adrenal cortex begins at the age of 6. While the secretion of GnRH, which is responsible for the onset of puberty, starts later. The reason for pubertal hair growth is an increase in the production of dehydroepiandrosterone (DHEA) and its DHEA-S by the adrenal glands, as well as delta-4-androstenedione, testosterone precursors that stimulate pubic and axillary hair growth. In girls, PA may be associated with excessive peripheral conversion of testosterone to dihydrotestosterone (increased aromatase activity). In the absence of other signs of androgenization of the body - acceleration of growth, maturation of the skeleton, pre-pubertal size of the uterus and ovaries, and in boys testicles, normal testosterone levels and moderately increased DHEA-S, the prognosis is favorable and sexual development does not deviate from the norm.
However, in some children, PA can be triggered by excessive production of ACTH (hydrocephalus, meningitis, etc.). There is more and more evidence of the association of PA with nonclassical forms of congenital adrenal cortex dysfunction (ADKD) and, in particular, deficiency of the enzyme 21-hydroxylase and, more rarely, 3β-hydroxysteroid dehydrogenase.
In the presence of a virilizing disease, clinical signs of androgenization appear: in girls - clitoral hypertrophy, high posterior perineal adhesion, hirsutism, development of the muscular system; in boys - a change in voice, an increase in the penis, activation of the sebaceous and sweat glands. These children experience accelerated growth and bone age.
Girls with premature adrenarche should be at risk of developing polycystic ovary syndrome. This group of patients requires corrective glucocorticoid therapy.
Differential diagnosis
Primary diagnosis is based on a thorough history and assessment of the degree of sexual development of the child according to the Tanner-Marshall classification. Early puberty in men in a maternal and paternal family is characteristic of testotoxicosis. The presence in the family of brothers with PMD or sisters with symptoms of virilization is more common with VDKN.
From the anamnesis it is necessary to find out the time of the appearance of secondary sexual characteristics, the speed of their progression. In girls, the degree of development of the mammary glands and areola, the condition of the skin, external genitals, and the presence of bloody discharge are assessed.
In boys - the degree of masculinization, the presence of hair on the pubis and armpits, the degree of change in the external genitals (the size of the penis, testicles).
Growth is assessed in both sexes by calculating the standard deviation coefficient (SD).
Early onset of the disease and rapid onset of symptoms are typical of testotoxicosis and hypothalamic hamartoma. Clinical symptoms of hypothyroidism, combined with PPR, suggest Van-Wyck-Grombach syndrome.
When indicating a history of congenital anomalies of the central nervous system, trauma, inflammation, one should think about the cerebral form of PPR.
Examination of bone age (radiograph of the hand), more than another indicator correlating with the stage of the child's sexual development, is mandatory for assessing the degree of PPD. If the bone age is more than 2 SD ahead of the passport age, this indicates an excess of sex steroids. A significant acceleration of bone maturation is characteristic of the central forms of PPR, as well as androgen-secreting adrenal tumors, VDKN. In isolated forms of PPR (premature thelarche and adrenarche), the bone age corresponds to the chronological one.
The tumor variant of cerebral PPR is excluded using computed tomography (CT) and magnetic resonance imaging (MRI). These research methods are included in the mandatory standard of the survey plan.
Pelvic ultrasound should be performed on all girls with suspected PPD. The size of the ovaries and uterus should be comparable to the level of sex hormones. Bilateral enlargement of the ovaries is a reliable sign of the central form of PPR.
Ovarian structure, follicular diameter, fundus to cervical ratio, uterine to endometrial length are important evaluative parameters, but many experts believe that they are not decisive in the differential diagnosis between PT and central forms of PPR. The ovaries can be asymmetrically enlarged in girls with peripheral PPR.
In boys, MRI or CT is preferable to detect adrenal masses.
To clarify the form of PPR, the levels of gonadotropic hormones, estrogens and androgens are determined. The levels of LH, FSH and estradiol reflect the state of the hypothalamic-pituitary-gonadal system, the concentration of DHEA and DHEA-S - the secretory activity of the adrenal glands.
For differential diagnosis between central and false forms of PPR, in all cases, a functional test with LH-RH should be performed. In true PPR, the diphereline test induces a pubertal response of LH and FSH. In children with peripheral forms of PPR, gonadotropins do not respond to stimulation.
An increase in DHEA-S is characteristic of premature adrenarche. An excess of adrenal androgens is possible with virilizing forms of VDKN, adrenal and ovarian tumors.
The tumor cause of PPR requires a study for the presence of AFP, beta-hCG, CEA.
Treatment
The main goal of PPR treatment is to eliminate the clinical symptoms of the disease, normalize the secretion of steroid hormones that accelerate bone maturation and close growth zones to achieve socially acceptable growth.
Treatment of true PPR involves blocking the pulsed secretion of LH-RH. The indication for the appointment of synthetic analogs of gonadoliberin is an early age and rapid dynamics of bone maturation. If the disease progresses slowly, this treatment should be approached with caution.
Triptorelin has been clinically tested in Russia. The drug is administered intramuscularly, the frequency of administration is 1 time every 28 days. Children weighing less than 20 kg - 1.875 mg, over 20 kg - 3.75 mg.
Normalization of the FSH level is noted after 3 weeks, a decrease in the size of the testicles and uterus from the 6th month of treatment. Inhibition of growth rate and skeletal maturation is observed by the end of the 1st year of treatment. The growth forecast is improving. The drug is well tolerated by patients. During treatment, constant monitoring of changes in bone age, growth rate, standard deviation coefficient (SDS) of growth is required.
The data confirm the feasibility of medication isolated thelarche against the background of a reduced thyroid function; in Van Wyck-Grombach syndrome, hormone replacement therapy with thyroid hormones is indicated. The criterion for the adequacy of treatment is the normal indication of TSH and free T4.
In McCune-Albright-Braitsev syndrome, pathogenetic therapy has not been developed. In cases of frequent massive bleeding, it is possible to use cyproterone in a daily dose of 70-100 mg. The drug has an antiproliferative effect on the endometrium, which leads to the cessation of menstruation. To reduce hyperestrogenemia, an inhibitor of aromatase activity is used - testolactone at a dose of 20-40 mg / kg per day or tamoxifen, which blocks estrogen receptors.
The tactics of treating testotoxicosis involves the appointment, firstly, of medroxyprogesterone (inhibition of testosterone synthesis), and secondly, ketoconazole (inhibition of the synthesis of hormones of the gonads and adrenal glands) or a combination of testolactone and spironolactone (inhibition of aromatase and blockade of androgen receptors). Ketoconazole is administered at a dose of 30 μg / kg per day per os. The use of the drug may be accompanied by adrenal insufficiency and liver dysfunction. With a late start of treatment, with a bone age of 12-13 years, a picture of true PPR may develop, in this case, therapy with synthetic analogues of LH-RH is performed.
Functional ovarian cysts in most cases undergo an independent regression within four months. When follicular cysts form in utero or in newborn girls, treatment is usually not carried out. Ovarian resection or laparoscopic peeling with suturing of the walls is performed if cysts with a diameter of more than 8 cm are detected.
Surgical methods of treatment are used in children with PPD developing against the background of hormonally active tumors of the adrenal glands, ovaries, and masses of the central nervous system; however, in some patients, removal of neoplasms does not lead to regression of PPR. The hypothalamic hamartoma is removed only for strict neurosurgical indications. In the presence of focal and general cerebral symptoms, surgery or radiation therapy corresponding to the type of tumor is performed. It must be remembered that radiation exposure or surgery on the bottom of the 3rd ventricle can provoke PPR. For this reason, such children should be constantly monitored by an endocrinologist. In cases where the leading clinical manifestation of the disease is only the symptoms of PPR, only conservative treatment is possible.
In girls with heterosexual premature puberty against the background of VDKN, if necessary, surgical correction of the external genital organs is performed. A penis-shaped or hypertrophied clitoris is recommended to be resected immediately after diagnosis, regardless of the child's age.
Further management of patients
All children diagnosed with precocious puberty should be constantly monitored (at least once every 3-6 months) before and throughout the entire period of physiological puberty. Treatment of true PPR with triptorelin is carried out continuously until the onset of puberty, since the cessation of its administration causes a resumption of the disease. The study of bone age is monitored with any form of PPD once a year.
Literature
- Prete G., Couto-Silva A., Trivin. C.et al. Idiopathic central precocious puberty in girls: presentation factors // PMC. 2008.
- Kobozeva N.V., Kuznetsova M.N., Gurkin Yu.A. Gynecology of children and adolescents. SPb, 1988.295 p.
- Dedov I.I., Semicheva T.V., Peterkova V.A. Sexual development of children: norm and pathology. M., 2002.232 p.
- Jospe N.Precocious Puberty. MD, 2012. www.merckmanuals.com.
- Kotwal N., Yanamandra U., Menon A. S.et al. Central precocious puberty due to hypothalamic hamartoma in a six-month-old infant girl // PMC. 2012.
- Upreti V., Bhansali A., Mukherjee K. K.et al. True precocious puberty with vision loss // PMC. 2009.
- Pagon R. A., Adam M. P., Bird T. D.et al. GeneReviews ™, Russell-Silver Syndrome. University of Washington, Seattle, 1993-2013.
- Stephen M. D., Zage P. E., Waguespack S. G. Gonadotropin-Dependent Precocious Puberty: Neoplastic Causes and Endocrine Considerations // PMC. 2011.
- Berberoglu M. Precocious Puberty and Normal Variant Puberty: Definition, etiology, diagnosis and current management // J Clin Res Pediatr Endocrinol. 2009, June, 1 (4): 164-174.
- Peterkova V.A., Semicheva T.V., Gorelyshev S.K., Lozovaya Yu.V.Premature sexual development. Clinic, diagnostics, treatment. A guide for doctors. M., 2013.40 p.
- Lowe L., Wong K. Premature sexual development in boys. www.urolog.kz.
- Lee P. Premature sexual development in girls. www.urolog.kz.
- Faizah M. Z., Zuhanis A. H., Rahmah R. et al. Precocious puberty in children: A review of imaging findings // PMC. 2012.
- Semicheva T.V. Premature sexual development (clinical, hormonal, molecular genetic aspects. Dis. Doctor of Medical Sciences. M., 1998.
- Bajpai A., Menon P. S. N. Contemporary issues in precocious puberty // PMC. 2011.
- Reisch N., Hogler W., Parajes S.et al. A diagnosis not to be missed: Non-classic steroid 11β-hydroxylase deficiency presenting with premature adrenarche and hirsutism // PMC. 2013.
- Precocious puberty By Mayo Clinic staff. 2011. www.mayoclinic.com.
V. V. Smirnov 1, doctor of Medical Sciences, Professor
A. A. Nakula
GBOU VPO RNIMU them. N.I. Pirogova, Ministry of Health of the Russian Federation,Moscow
Abstract. Precocious sexual development is the frequent violation of puberty in children and in their etiology and pathogenesis is a heterogeneous disease. The article summarizes the current data on the causes of violations of formation of the hypothalamic-pituitary-gonadal relationships cause premature sexual development. A classification of diagnosis and treatment of this pathology.
- True forms.
- For girls:
- enlargement of the mammary glands;
- pubic hair;
- acne (blackheads);
- menstruation that is regular. However, more often in girls with true premature puberty, menstruation may be absent for 5-6 years after the onset of secondary sexual characteristics.
- Boys:
- testicles and penis increase in size;
- acne, increased sweating, a specific pungent smell of sweat appear;
- sexual hair growth;
- the voice becomes coarse, muscle mass increases.
- For girls:
- False forms.
- For girls:
- menstruation begins simultaneously with the enlargement of the mammary glands. The discharge is random, can be profuse or "smearing";
- isolated thelarche (premature enlargement of the mammary glands) is the only secondary sex characteristic in girls under 2 years old;
- isolated adrenarche (pubic hair growth in girls from 3 to 8 years old, not combined with the development of other signs of puberty).
- Boys:
- progression of secondary sexual characteristics;
- the pre-pubertal (before puberty) volume of the testicles remains.
- For girls:
Forms
- True, or central- due to the premature activity of the hypothalamic-pituitary system (the area of \u200b\u200bthe brain that regulates the activity of the endocrine glands). An increase in the production of sex hormones by the gonads in this case is a consequence of the stimulation of the internal gonads by gonadotropins (pituitary hormones (areas of the brain) that regulate the work of the gonads).
- False, or peripheral - due to the premature production of sex hormones by tumors of the gonads or adrenal glands, independent of the production of gonadotropins.
- Gonadotropin-independent- premature sexual development, in which the activation of the activity of the gonads is caused by genetic disorders.
- complete - an increase in the mammary glands in girls, the penis and testicles in boys, hair growth in the armpits, pubic region, a change in the timbre of the voice, the formation of a female figure in girls (breast augmentation, hips) and in a male - in boys (an increase in the width of the shoulder girdle, reduction of fat deposition on the buttocks), acceleration of growth;
- partial, or incomplete- characterized by the isolated development of hair growth in the axillary and pubic areas (premature pubarche) and isolated enlargement of the mammary glands (premature thelarche).
The reasons
- Causes of true premature puberty.
- Tumors of the central nervous system.
- Non-neoplastic brain damage (eg, birth injury, meningitis (inflammation of the meninges)).
- Congenital syndromes:
- type 1 neurofibromatosis (hereditary disease that predisposes to the onset of tumors of the nervous system);
- russell-Silver syndrome (a syndrome accompanied by moderate production of gonadotropins (hormones that regulate the functioning of the gonads) from early childhood);
- vanVijk-Grumbach syndrome (develops in children with primary hypothyroidism (low levels of thyroid hormones)).
- True precocious puberty with prolonged exposure to sex hormones.
- Idiopathic (the exact cause of premature puberty has not been established).
- False premature puberty.
- Boys:
- testicular tumors (leydigomas);
- adrenal tumors (androsteromas);
- congenital dysfunction of the adrenal cortex (changes in the body that develop with excess production of androgens (male sex hormones) or estrogens (female sex hormones) by the adrenal cortex).
- For girls:
- ovarian tumors;
- adrenal tumors;
- ovarian cysts.
- Boys:
- Gonadotropin-independent forms:
- mcCune-Albright-Braitsev syndrome (premature puberty occurs as a result of a congenital gene mutation, which causes an uncontrollable activation of estrogen production (increases the production of female sex hormones));
- testotoxicosis (activation of testicular function without the participation of gonadotropins (hormones that regulate the work of the gonads)).
Diagnostics
- Analysis of complaints and anamnesis of the disease, general examination.
- Early onset of puberty (8-9 years):
- enlargement of the mammary glands in girls;
- menses;
- an increase in the size of the testicles and penis;
- sexual hair growth;
- the voice becomes coarse, muscle mass increases;
- acne (blackheads);
- acceleration of growth up to 10-15 cm per year.
- Comparison of the degree of physical and puberty according to Tanner (a scale describing the puberty of children, adolescents. Tanner's stages are based on the observation of changes in external primary and secondary sexual characteristics: changes in breast size, male and female genital organs, development of pubic hair) with age standards.
- Early onset of puberty (8-9 years):
- Laboratory and instrumental research methods.
- Determination of the level of follicle-stimulating and luteinizing hormones (hormones necessary for normal reproductive function).
- Determination of levels of prolactin, thyroid-stimulating hormone (pituitary hormones).
- Determination of levels of estradiol (female sex hormone), testosterone (male sex hormone), cortisol (adrenal hormone), 17-OH-progesterone (intermediate in the synthesis of cortisol), dehydroepiandrosterone sulfate (adrenal hormone), free thyroxine and triiodothyronine.
- Conducting tests that stimulate and suppress the production of steroid hormones:
- a test with a synthetic analogue of gonadotropin-releasing hormone (a hormone that regulates the synthesis of follicle-stimulating and luteinizing hormones);
- a small test with glucocorticoids is performed in girls with premature pubarche (hair growth of the pubic region) when an increased content of 17-OH-progesterone and / or dehydroepiandrosterone sulfate and testosterone in the blood is detected. Normally, there is a decrease in the level of 17-OH-progesterone, dehydroepiandrosterone sulfate and testosteronan by 50% or more. The lack of dynamics in the concentration of hormones suggests the presence of an androgen-producing tumor.
- Ultrasound of internal genital organs with an assessment of the degree of maturity of the uterus and ovaries in girls.
- Ultrasound of the mammary glands, thyroid gland and adrenal glands.
- Radiography of the hand and wrist joint to determine the biological age of the child.
- Electroencephalographic and echoencephalographic study with the identification of nonspecific changes (the appearance of a pathological rhythm, increased convulsive readiness), most often accompanying premature puberty against the background of disorders of the central nervous system.
- Magnetic resonance imaging (MRI) of the brain in order to exclude masses of the brain.
- CT, MRI of the adrenal glands to exclude masses.
- Molecular genetic testing to detect genetic mutations.
- Consultation is also possible, (for girls), (for boys).
Treatment for premature sexual development
- Gonadotropin-dependent premature puberty:
- long-acting analogues of gonadotropin-releasing hormone (a hormone that regulates the functioning of the reproductive system);
- progestogens are used to prevent uterine bleeding in girls.
- Gonadotropin-independent premature puberty (isosexual), premature isolated thelarche (enlargement of the mammary glands). The annual observation and temporary abstinence from vaccinations in girls with premature thelarche are shown, taking into account the possibility of enlargement of the mammary glands after their implementation.
- Premature pubarche (pubic hair). They carry out preventive measures aimed at forming a stereotype of a healthy diet and preventing weight gain:
- reduction in the diet of foods high in carbohydrates (sugar, candy, jam) and fats (butter, fatty meat, lard);
- regular exercise;
- compliance with the duration of a night's sleep at least 8 hours.
- Gonadotropin-independent precocious puberty (heterosexual): glucocorticoids (adrenal hormones).
- Surgical methods of treatment are used in children with premature sexual development, developing against the background of hormone-active tumors of the adrenal glands, ovaries, as well as masses of the brain (removal of neoplasms).
Complications and consequences
In the absence of treatment:
- infertility (in the future);
- osteoporosis (decreased bone density);
- increased arterial (blood) pressure;
- obesity;
- psychological complexes among peers due to the early development of secondary sexual characteristics (breast enlargement in girls, hair growth in the armpits and face in boys, etc.);
- patients with neoplasms have a high risk of malignancy (transformation into cancer) of tumors. Irradiation of intracranial tumors can lead to the development of pituitary insufficiency (a disease that develops as a result of a violation of the secretion of pituitary hormones (the area of \u200b\u200bthe brain that regulates the activity of the endocrine glands), which is manifested by a deficiency in the function of the organs of the peripheral endocrine system (thyroid gland, adrenal glands, gonads)).
They say about the premature sexual development of girls when they have sexual characteristics up to 7 years old - the mammary glands grow, hair is noticeable on the pubis and armpits, while female forms begin to form actively. In addition, the girl has an early period. This process is not the norm. Puberty should occur from 12 to 14 years old, a year of difference is allowed. If mothers notice all the signs in little girls, it is worth being examined to prevent different consequences.
Symptoms
One can suspect something was wrong by the following signs: in little girls who have not yet even turned 7 years old, their hips are noticeably rounded, an hourglass figure is noticeable, irregular menstruation occurs, while the child's growth is slowed down.
In medicine, such forms of the disease are distinguished.
True sexual development
It is provoked by an increased production of hormones - the pituitary gland, the hypothalamus, which stimulate the work of the girl's ovaries. In the case of full true sexual development, the girl develops all the symptoms described above. If the child has an incomplete true form, the signs are still the same, only periods begin to go from the age of 10.
Ovarian sexual development
The problem is associated with increased production of sex hormones. In this case, only disruptions in menstruation are of concern, while other signs do not appear.
Hereditary form
The girl has no health problems at all, only puberty occurs 2 years earlier than her peers: the first menstruation appears, the mammary glands grow faster.
Heterosexual form
One of the unpleasant pathologies in which a girl begins to develop sexual characteristics characteristic of men. Puberty here is associated with an increased amount of male hormones; it can still begin in utero. A girl may have male-type external genitalia, while there is a uterus, ovaries. This pathology is explained by adrenogenital syndrome - adrenal disease.
The reasons
Most often, pathology is associated with heredity, it is transmitted from mother to daughter. If so, the girl will not have impaired fertility. It is more dangerous when the disease is associated with disorders of the pituitary gland, hypothalamus, hormonal excess. The main factors include:
- Consequence of traumatic brain injury.
- Congenital structure of the brain.
- Complication after the transferred virus, bacterial infection.
- A brain tumor.
- Poisoning with poisons.
- Radiation therapy.
- Cyst, ovarian cancer.
As a rule, girls have problems with puberty if their mother, during pregnancy:
- I used drugs, alcohol.
- She suffered from endocrine disorders.
Diagnostics
The doctor always collects a medical history, finds out when the first menstruation began, what kind of discharge the girl has. He is also interested in when the breast began to grow, the first pubic hair appeared.
Then the doctor analyzes the genetic predisposition. The doctor asks who had violations of this nature - grandmothers, sisters, mothers or aunts, cousins.
Mom's medical history is also important. The doctor asks her about the past gynecological diseases, operations, as well as about the number of abortions, pregnancies.
After the interview, the doctor examines the child, feels the genitals, he is interested in the ovaries, cervix, size, and the presence of painful sensations. During a general examination, attention is paid to secondary sexual characteristics:
- Body type.
- Striae.
- Hair growth.
- Discharge from the nipples.
- How the mammary glands develop, is there any discharge from the nipples.
It is important for the doctor to determine the bone age for this, an x-ray is prescribed. This survey provides an opportunity to learn about age-related disorders. An analysis for hormones is also important. Most of all it is drawn to sex hormones, pituitary gland, adrenal hormones. An x-ray of the skull may be taken to find out if there is a tumor in the hypothalamus, pituitary gland.
To exclude anatomical abnormalities of the brain, MRI is prescribed. In addition, the girl must undergo an ultrasound of the female organs, where it is carefully checked whether there are abnormalities of the genital organs, cysts, or a tumor.
In severe cases, laparoscopy is prescribed using an endoscope. This examination is necessary to check the fallopian tubes, uterus, and ovaries. If cancer is suspected, a biopsy may be done, during which samples of ovarian tissue are examined.
Important! In addition to the gynecologist, the girl is examined by an endocrinologist.
Treatment methods
The course of therapy depends on the cause of the premature sexual development. Recommended:
- A diet that can help you regain weight.
- Consultation with a psychotherapist, taking sedatives.
- Taking medications to reduce pituitary production. After taking the drug, the ovaries do not mature so quickly and actively work, thus slowing down sexual development. If you stop taking the medicine, maturation is reactivated.
- Operation in case of diagnostics of tumors of the ovaries, pituitary gland, adrenal glands, hypothalamus, as well as congenital anomalies.
Important! The hereditary form is not treated, but the girl should be registered with a gynecologist, always under supervision.
Effects
If you do not start treating the child in a timely manner, everything will end:
- Low growth.
- Changes in body proportions - short legs, arms, long body, broad chest.
Most often, sexual dysfunctions are associated with pathology of the ovaries, brain, adrenal glands, therefore, timely diagnosis and treatment is necessary.
Prevention
It is easier to prevent pathology than to watch your child suffer, so stick to these rules:
- Monitor the girl's diet. In her diet should be foods rich in fiber - fruits, vegetables, herbs. Do not give your child fried, hot, canned, spicy foods.
- Regularly observe the newborn baby with a pediatrician, endocrinologist.
Monitor your child's health carefully!
Why do children sometimes enter puberty much earlier than their peers? Doctors and a psychologist shared their views.
Modern children grow up earlier, this fact is noted by many doctors. But what does premature sexual development mean, how does it happen, what features should parents pay attention to?
These and many other questions were answered by several experts at once: a gynecologist, endocrinologists and a psychologist.
Elena Alexandrovna Pisareva
What is considered early puberty
Early or premature puberty is understood as the appearance of secondary sexual characteristics in girls before 8 years old, in boys before 9 years old.
Secondary sexual characteristics are an increase in the mammary glands (in girls) and an increase in the volume of the testicles (more than 4 ml) and the size of the genitals (in boys), the appearance of pubic and axillary hair. There may be an early appearance of one or more components.
The cause of premature puberty may be early activation of the production of sex hormones.
There are two conditional groups.
The first includes states when the appearance of signs of early maturation is temporary and passes on its own without our intervention. It is not considered a pathology and does not require treatment.
For example, there is often a condition when girls in the first years of life have an enlargement of the mammary glands, the so-called "isolated thelarche", which later goes away.
The second group includes conditions when the production of sex hormones started ahead of time and will not stop without treatment, and signs of puberty will progress.
To understand which option we are dealing with and whether treatment is necessary, you need to undergo a specialized examination and contact a pediatric endocrinologist.
Can we say that this is a modern trend
There have always been problems with early puberty. They are more common among girls. There is evidence of earlier puberty in children living in the southern regions, but even among them, early puberty can be pathological.
How does this affect the growth of the child
With early puberty, growth rates accelerate, and children with this condition tend to be taller than their peers. However, due to the excessive production of sex hormones, the growth zones are closed very quickly, and as a result, the child may be short relative to his peers.
With closed growth zones, we cannot change the height of the child.
Also, with early puberty, given the increased secretion of hormones, social maladjustment of the child is possible.
Is it inherited
Early puberty is usually not hereditary. In world practice, only a few cases with inheritance in the family are known.
Advice to parents
If you notice the early appearance of secondary sexual characteristics, which were mentioned above, you need to contact a pediatric endocrinologist to clarify the reasons and determine the need for treatment or, possibly, the choice of observational tactics.
By the time of admission, be sure to prepare growth indicators for previous periods of observation so that the doctor can assess the dynamics of development.
Comments Natalya Aleksandrovna Chekenova, gynecologist-endocrinologist, pediatric gynecologist, reproductologist, doctor of ultrasound diagnostics (14 years of experience)
Natalya Alexandrovna Chekenova
Causes of early sexual development
Violation of sexual development, like any pathological condition, cannot arise just like that. This can be preceded by many factors, such as:
⁃ chronic intrauterine fetal hypoxia;
⁃ acute hypoxia during childbirth;
⁃ craniocerebral trauma in a child at any age;
⁃ tumors of the central nervous system;
⁃ tumors and hyperplasia of the adrenal glands;
⁃ tumors and dysfunction of the gonads;
⁃ thyroid disease (primary hypothyroidism);
⁃ congenital genetic pathology (Russell-Silver, McCune-Albright-Braitsev syndromes).
If suddenly you realize that your child began to grow and mature faster than all peers - the girls began to grow mammary glands, hair, behavior changed, menstruation began; the boys have an increase in the genitals, hair growth, coarsening of the voice, polyuts, which means it is time to see a doctor.
The deeper and more severe lesions the child has, the more severe and earlier the manifestations will be.
Condition diagnostics
First of all, the specialist needs to obtain important information about the child's health:
⁃ collecting anamnesis (how pregnancy and childbirth began and proceeded);
⁃ examination of the child;
⁃ blood chemistry;
⁃ blood hormones;
⁃ functional tests (with gonadotropins);
⁃ genetic research;
⁃ Ultrasound of genitals, adrenal glands, brain;
⁃ electroencephalography;
⁃ X-ray of the hands;
⁃ MRI, etc.
The child must be examined by narrow specialists. After that, the doctor will be ready to decide on the tactics of treatment. Sometimes this requires more frequent monitoring, and sometimes correction with serious drugs, surgical treatment.
Julia A. Galkina
What other factors affect sexual development
The physiological development of a person occurs individually for everyone. It is associated with the following factors:
hereditary (how his parents, grandmothers, grandfathers, brothers, sisters developed);
ethnic (features of development among different nationalities);
socio-economic (in what conditions a person develops, his standard of living);
food factors (dietary habits, dietary habits);
climatic conditions of the living environment;
the presence of various chronic diseases of the endocrine system (dysfunction of the thyroid gland, adrenal glands, pathology of the ovaries, testicles) and the intake of hormonal drugs.
When assessing sexual development, it is necessary to take into account the nationality of the child, belonging to a particular race, climatic and social conditions of his residence.
For central Russia, the beginning of puberty (puberty) in boys is 9-14 years old, in girls 8-13 years old.
In peoples living in hot climates, puberty of children occurs earlier.
But there is also a hereditary predisposition for the onset of puberty, therefore, the age of its onset in parents, and possibly in grandmothers and grandfathers, is taken into account.
What are the signs that parents can understand that development is premature?
It is possible to suspect early sexual development in a child already with visible changes in his body that are not typical for his peers:
a leap in growth of more than 10-12 cm per year, which may be accompanied by weight gain;
hair growth in the armpits, pubic hair;
increased greasiness of the scalp and hair;
increased sweating, the smell of sweat may change;
acne rash, seborrhea of \u200b\u200bthe scalp;
in girls: enlargement of the mammary glands, darkening of the nipple halo, the formation of a more feminine figure (appearance of the waist, enlargement of the hips), the appearance of menstruation.
If sexual development begins ahead of time, the child's body is not ready for the appearance of so many hormones.
He does not have psychological adaptation. Often these children experience peer ridicule. They can withdraw into themselves, experience a sharp change in mood, hysteria, aggression. Subsequently, there may be a violation of sexual behavior.
Which doctors should you contact
In each case, the cause of premature sexual development is individual. It is not an independent pathology, but arises as a result of the manifestation of certain diseases in children under 6-7 years old. Therefore, examination by a number of specialists is required: a pediatrician, a pediatric endocrinologist, a pediatric gynecologist, a neuropathologist, an ophthalmologist.
I also recommend undergoing the following examinations: blood test for hormones (LH, FSH, estradiol, prolactin, TSH, free T3, free T4, cortisol, testosterone, 17-OH progesterone, DEA-c), MRI of the brain (to exclude brain tumors brain, cysts, hydrocephalus), CT or MRI of the kidneys and adrenal glands (to exclude an increase in the adrenal glands, tumors), ultrasound of the pelvic organs (to exclude cysts, ovarian tumors, adenomatous nodes), as well as assess bone age.
Victoria Romanova, a practicing psychologist, a leading trainer of the ALMA Academy, a female trainer, a life coach, a master of the Indo-Tibetan method of treatment
Victoria Romanova
Today's adolescents are growing up earlier than their parents once did, both physically and mentally. Here's what parents need to know.
Physiological and psychological maturation of the child
From a physiological point of view, early puberty is expressed in the formation of secondary sexual characteristics: the genitals increase, the active growth of body hair begins, in girls - the growth of the breasts.
Normally, these processes occur when the child reaches 10 years old.
If secondary sexual characteristics appear earlier, then it is best to consult a doctor to rule out possible diseases of the brain or hormonal system of the body.
Psychologically, early puberty in children consists of three phases: autosexuality, homosexuality and heterosexuality. You need to understand that every child passes them, regardless of gender, race, religious or other beliefs of the parents.
Only the correct attitude of adults to this process will help the correct formation of sexuality in a child.
Let us dwell on these stages in more detail.
Autosexuality
Autosexuality is expressed in the fact that the child begins to explore his body, touch it, play with the genitals. The kid does not see anything bad or shameful in this, for him this is only the stage of getting to know his own body, and globally - the initial phase of the formation of his sexuality.
At this moment, the main task of the parents is not to scare the child, not to shame, and even more so not to punish him for excessive interest in some parts of the body.
On the contrary, you need to unobtrusively explain to the kid how boys and girls work, without going into unnecessary details. To help moms and dads - a huge amount of children's literature on this topic with vivid illustrations that are understandable to a child of any age.
However, more often than not, parents raised in severity and themselves sexually illiterate begin to panic. It seems to them that such games indicate the abnormality of the baby. They punish the child, forbid him to touch himself, shout. As a result, the baby feels bad, spoiled, unworthy of the love of mom and dad.
Ultimately, all this leads to serious problems in the sex life of a grown child.
As a rule, children whose parents prevented them from going through the phase of autosexuality are guided by the satisfaction of only their own needs.
Sex for them is just a mechanical process of self-gratification. Masturbation becomes the only source of sexual satisfaction, even during sex with a partner. Such people are unhappy in their personal life, it is difficult for them to find a soul mate, they cannot please their partner.
Homosexuality
If the child has moved to the homosexual phase of sexual development, it means that his parents did everything right at the first stage. The second phase is as natural as the first.
Puberty is structured from simple to complex. First, the child learns the simplest and most accessible "material" for him - his own body. Then - an identical body, but already of a different person. And only after that - the body of a person of the opposite sex.
This is why there is nothing dangerous about the homosexual developmental stage of children.
It is very difficult for parents to go through this stage and adequately respond to the child's behavior. They try to prohibit such contacts, punish children, condemn them.
At the same time, society itself creates the prerequisites for homosexuality, dividing the younger generation by gender in everyday life. These are sports clubs only for boys or only for girls, and closed educational institutions where children of different sexes do not study together, and much more.
But it is the constant bans on communicating with members of the same gender that provoke a teenager to rebellion.
As a result, he does not go through the stage of homosexuality and can "get stuck" in it for life.
Parents should treat the child with understanding, talk a lot with him about everything that worries him. If adults are "old school" and it is difficult for them to conduct such conversations, then you need to turn to competent psychologists who will help the teenager move to the heterosexual stage of sexual development.
Heterosexuality
If both initial phases of puberty are successful and adults do not interfere with the natural formation of the child's sexuality, then he enters the phase of heterosexuality.
It is characterized by interest in the opposite sex, the formation of sexual desire. At this stage, adolescents begin to comprehend the characteristics of the opposite sex, learn about love and harmony in relationships. This is the final point in the formation of healthy sexuality.
Photo: Shutterstock.com Let's be friends on social networks! Subscribe to us on Facebook, VKontakte and Odnoklassniki!